-

Pathology Network LIMS System Interoperability Redesign
-

Virtual Wards Performance Evaluation & Re-Design
-

Health on the High Street
-

Workforce Profiling for National Genomics Service
-

Diagnostic Transformation Team Options Appraisal
-

Genomics Strategic Demand and Capacity Modelling
-

Enabling a Productivity Shift in Mental Health
-

Transforming Inventory Management at Cambridge University Hospital
-

Accelerating Scan4Safety Agenda through Inventory Management Optimisation
-

Overcoming the barriers to developing future-ready community diagnostic services
-

New Statesman Future of Healthcare Conference
-

Enabling ICB Elective Recovery Through Workforce Modelling
-

ICS Collaborative Operating Model and Commercial Efficiency
-

Supporting Sustainability and Social Value in Estates and Facilities
-

How can systems integrate their estates and facilities services?
-

What now for NHS infrastructure
-

Financial Improvement: Targeting at ICB level through Population Health Management
-

NHS Workforce Plan: Translating national targets at a local level through productivity and retention
-

Financial Improvement Plans: Schemes to Target Outcomes
-

Financial Improvement Plans: From Quick Wins to Strategic Programmes
-

The status of virtual wards across England
-

Establishing a Remote Diagnostic Hub
-

Non-Patient Transport Service Review & Optimisation
-

Case for Regional Aseptic Services in Yorkshire
-

Regional Technical Services Strategy
-

Saying Goodbye to Category Tower 8
-

Integrated Care Strategies: Turning rhetoric into reality
-

Commercial Case for NHSE South-West Community Diagnostic Hubs
-
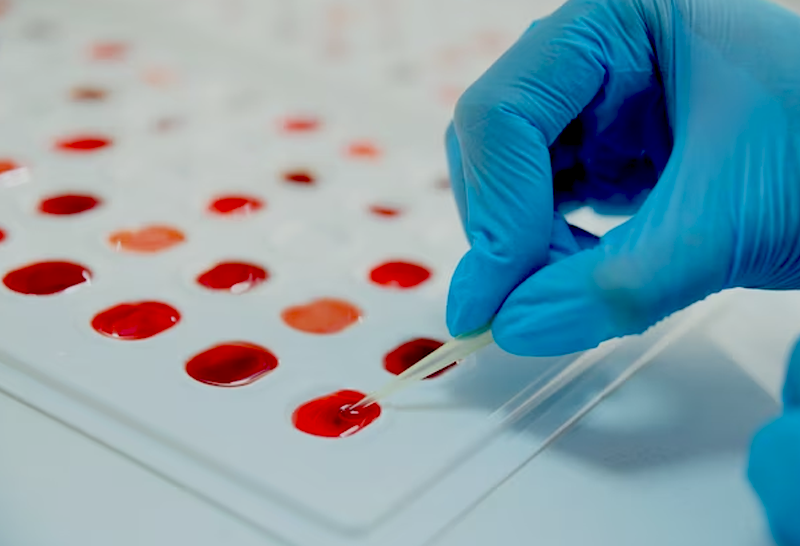
Contracting for Sample Processing in Health Research
-

Healthcare on the High Street – Research Diagnostic Facility
-

Delivery of a National Category Management Service
-

Multi-Trust Urgent and Emergency Care Facility Business Case
-

Pro-bono COVID-19 Grant Application Support to Homerton Healthcare
-

Delivering improvements to discharge practices
-
Virtual Wards: First-of-kind Case Study on Heart Failure
-

Technology-enabled virtual wards the future of healthcare
-

Discharge to Assess: Where the rubber hits the road
-

Transforming homes into hospitals
-
Technology-enabled Virtual Wards
-

Client Testimonial: Lancashire and South Cumbria Health and Care Partnership
-

Logistics Management for a Global Pharmaceutical Company
-

Patient Safety Business Case Development
-

Creating more effective Estates and Facilities strategies
-

Preparing for the challenges of tomorrow with robust continuity planning
-

Reshaping long neglected sterilisation services
-

Implementation of a Trust-wide Patient Safety Programme
-

Redesigning a one-of-a-kind NHS shared service facility
-

Delivering a value assessment for regional health and social care collaboration
-

Private Provider Value Assessment
-

Facilities Management Cost Reduction
-

Diagnostics Laboratory Cost Reduction Programme
-

Optimisation of Diagnostic Specimen Collection Network
