Content
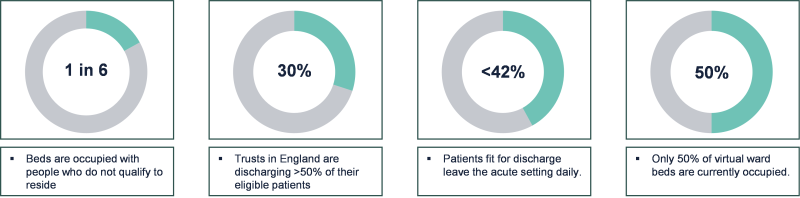
“Virtual wards” are a key initiative across health and social care to help keep people at home, or to get them back to their usual place of residence after a hospital spell. The issues of bed occupancy in acute trusts are well-known (see the figure below), as is the imperative to look after people well to prevent deterioration wherever possible and avoid a trip to hospital. The use of the name “ward”, therefore, is slightly misleading as it suggests hospital-type care whereas the gains are at least as great in admission avoidance and the maintenance of health. The word “virtual” also has negative connotations (suggesting that care is less immediate or personal) but, for the purposes of this paper, we’ll use the current expression whilst appreciating its potential breadth of meaning.
The idea is not new (it was first developed about 20 years ago) but the current interest from digital and technology providers, together with significant amounts of funding (£450m over the last 2 years), has led to their adoption accelerating over the last 2 years. In principle, it has multiple benefits over the long term:
- It generates better outcomes for patients (being at home keeps people healthy and aids recovery, relative to being in an acute setting);
- It is a much better experience for patients, carers and clinicians (in general, people would prefer to be at home surrounded by family and familiar surroundings, knowing that you can access support as and when you need it)
- It makes better use of clinical resource (more attention in hospitals can be spent on those who need it), and is more financially efficient (the cost of running a virtual ward is much cheaper than that of a physical hospital ward).
Through the Spring of 2023, Akeso conducted research across all trusts within England in order to understand how widespread the adoption of virtual wards has been and whether they are having the predicted impact. In this first article, we present the current state of coverage across the country. 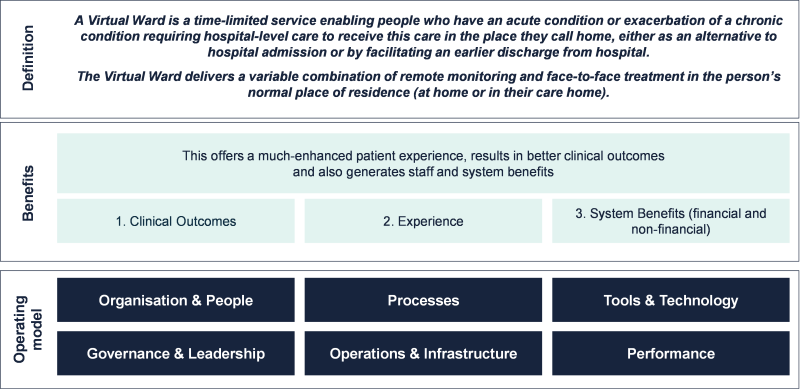
Through the Spring of 2023, Akeso conducted research across all trusts within England in order to understand how widespread the adoption of virtual wards has been and whether they are having the predicted impact across all domains. In this first article, we present the current state of coverage across the country.
The rule of two-thirds
For completeness, all 240 trusts in England were invited to contribute to a survey which aimed to capture a snapshot of the state of the virtual ward programme across England. These included large acute trusts (for which the relative share of potential virtual ward beds was large, given their catchment and coverage), specialist trusts, and community trusts. The trusts were separated into 4 categories: category 1 trusts were the largest trusts in the country who, between them, would cover about 50% of all potential virtual ward beds1; categories 2-4 trusts had smaller proportions (approximately 30%, 15% and 5% respectively).
Over 2 months, responses were received from over 160 – about 2/3rds of all trusts within England – which is sufficient to make projections about the overall state across the nation.
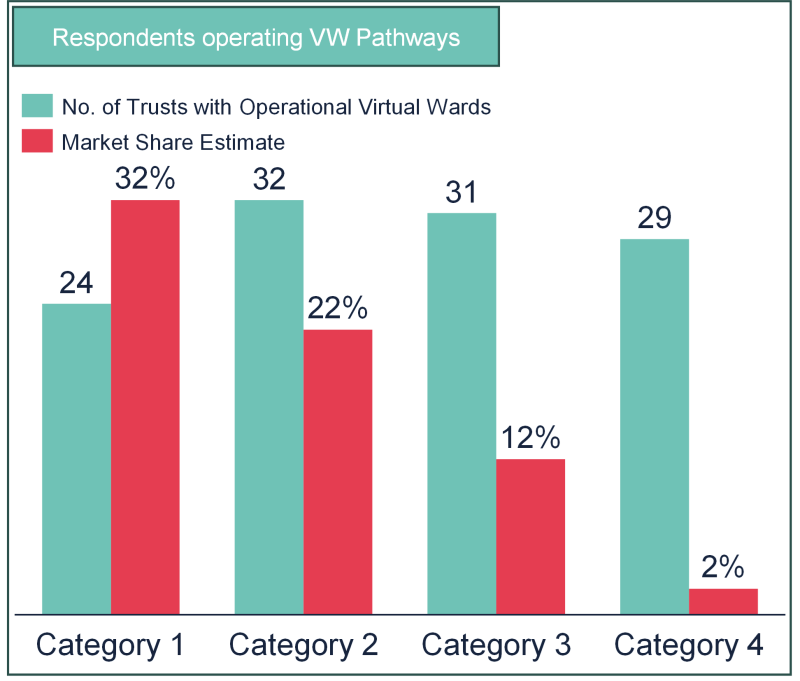
Adoption: Encouragingly, every one of the category one trusts who responded said they had virtual ward pathways in place. Perhaps more surprisingly, even 90% of the category 2-4 trusts who responded also indicated that they also have pathways in place. There was no correlation between adoption and CQC rating – the adoption of virtual wards was similar across all four ratings categories.
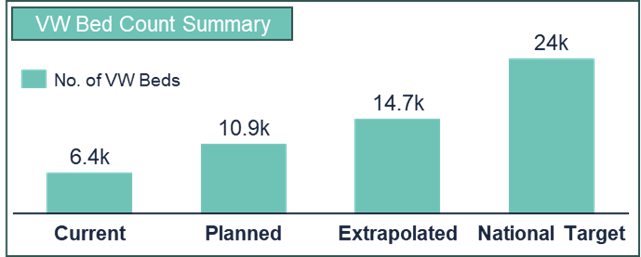
Coverage: Coverage: So, if almost everyone has some form of virtual ward offering, how significant is their capacity? Our respondents between them have about 6,500 virtual ward beds open at the moment; and the average number of virtual ward beds available is 50-60 (the equivalent of a couple of physical wards). This number is likely to almost double by the end of 2023/24 (likely before Winter pressures hit) to a figure of nearly 11,000, as plans for the rest of the year are delivered. If this figure were replicated across all trusts across the country, the number of virtual ward beds which will be open by the end of the year will hit nearly 15,000. Progress is good and will continue to be positive, therefore, but it’s most likely that the total number of virtual ward beds open by the end of this year will fall significantly below NHS England target of 24,000 (which corresponds to about 40 beds per 100k head of population in England). Again, the proportion is about 2/3rds.
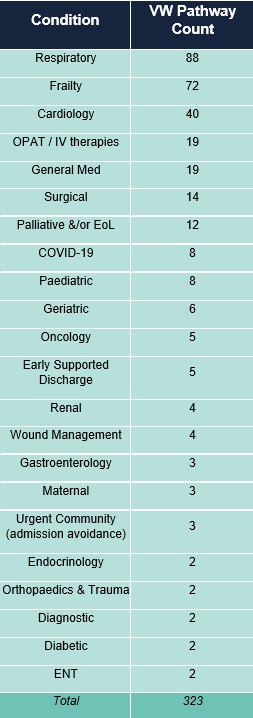
Specialty representation: Building on the capacity analysis, what are the beds being used for. Much of the existing literature on good virtual ward case studies points to a predominance of respiratory and cardio-vascular pathways. The responses confirm this: of the 300+ pathways that were identified as being available across trusts which responded, the top three were indeed respiratory, general frailty, and cardiology. Again, these made up about 2/3rds of all available pathways. However, there were a total of 33 different pathways listed, including diagnostic and maternity pathways, which indicates the growing spread of virtual wards to very many clinical areas. It is worth noting that, whilst surgery, cancer, paediatrics and women’s health were all represented, the majority of the pathways were related to medical specialties.
Technology: given the increased comfort with remote and digital technology platforms in facilitating clinical services, it was no surprise to find that there was a plethora of private technology companies who are assisting trusts of all sizes with the adoption of virtual wards. 13 different companies were named specifically, and often trusts were engaging multiple technology providers who delivered different pathways, depending on their clinical efficacy. We think this is an under-representation of the range of technology providers who are involved – many smaller trusts listed large acute trusts as their partner and, thus, may not have been aware of the supporting technology provider.
Summary
Progress in the roll-out of virtual wards has been positive, with 15,000 such beds likely to be open by the end of the year. The funding which has been made available has undoubtedly helped and it is very encouraging to see the range of different pathways which are represented. As is the way with innovation and adoption, using local workforce to figure out what works locally leads to solutions which are likely to succeed – this is not a simple exercise in “plug-and-play” the latest digital between the EPR and iPhones. Time, space and resources will continue to be needed so that learning is made and adoption sustained.
In the long term, virtual wards have to show benefits for patients and carers (in terms of experience and health outcomes), staff (in terms of working conditions and job satisfaction) and efficiency in terms of use of capacity (both physical space and the valuable workforce). At the moment, whilst beds are open, their occupancy is actually relatively low, and there is very little evidence that sustainable impact is being made – over time, it should be easy to see that admissions are falling, acute-based length of stay in decreasing, and that staff are being better used (and happier in their jobs). For this to happen, there are a number of factors across six operating model domains which need to be in place. Our next article in this series will dig deeper into a number of these to unearth further promising progress.
We continue to work with NHS and partners alike to learn and spread best practice in virtual wards to improve services for patients, carers and staff alike.

