In the first article of Akeso’s financial improvement series, we set the scene on the financial challenge faced by NHS organisations and Integrated Care Boards (ICBs) and outlined the opportunities to leverage tangible savings within differing time horizons.
In this article, we share examples of the proven efficiency and savings schemes that Akeso have supported our clients to implement, which also address clinical, operational, and patient challenges.
Short-term
Quick-win initiatives with in-year benefits realisation, and tactical savings in as little as 3 to 6 months:

Controlling costs by reducing the use of inappropriate products and services, whilst finding feasible ways to change spend patterns throughout the organisation is key to managing demand. Additionally, implementation of robust stock management principles reduces excess stock and releases clinical time to care, whilst ensuring staff have the correct type and number of items at the correct time for safe and effective care delivery.

Conducting detailed reviews with budget holder input to identify all types of discretionary spend. Outputs from reviews support data-informed decisions to implement the necessary controls, governance, and tracking across organisations. For example, highlighting inflated contract spend for renegotiation, and non-essential ad-hoc spend.
Clinicians should also be engaged to develop an exclusion list to protect budgets, where necessary

At a provider level, implementing process improvement to focus on reducing agency spend. At a system level, partners working collaboratively to operate joint banks, aligning agency rates across the system, and sharing specialised clinical resource, rather than competing to recruit from the same pool.
Reducing expenditure on non-clinical staffing should be a priority.
Medium-term
Schemes delivering within one to two years:

Use of data, technology, and digitalisation to automate processes, reduce administrative burden, and provide care closer to home, whilst releasing staff time and resources through:
- Robotic Process Automation (RPA) for both front office activities, for example patient administration, and corporate services, for example Finance and HR systems.
- Inventory Management and Point of Care solutions. A recent NHS Supply Chain (NHSSC)review found ‘improved inventory management represents the most significant cash-releasing saving and operational efficiency available in supply chain management within the NHS’[1].

Implementing best practice initiatives, such as improved discharge planning, to reduce length of stay, release of escalation beds, and increase income through delivery of more elective operations.
Akeso have a Discharge to Assess (D2A) and community support maturity matrix that helps acute Trusts, local authorities and ICBs to understand the fundamental requirements for D2A to be a success[2].
Out-of-hospital programmes, including virtual wards and remote monitoring, enable release of bed days and improve patient outcomes through admission avoidance and delayed discharges, supported by a well-defined benefits framework[3].
Virtual ward schemes are essential if we are to meet the national target of 50 Virtual Wards per 100,000 population.

At a provider level, informed by Getting it Right First Time (GIRFT) benchmarking, the focus is on improving productivity through booking procedures, scheduling, and improving staff skill mix.
At a system level, supporting providers in moving procedures to the most appropriate setting, e.g., from traditional theatres to community and outpatient settings, as well maximising the use of digital tools for virtual care, where appropriate.
Long-term
Opportunities to realise savings after two years, with strategic programmes delivering five years and beyond.

Population Health Management analytics and benchmarking support optimisation of resources and best-practice clinically led care across pathways. Examples include:
- Innovative cross-pathway workforce models such as use of advanced practitioners and nursing staff in the community and acute settings, recognising current recruitment constraints.
- Improving workforce productivity and elective recovery by using analytical tools to understand, predict and plan for system-wide capacity and demand.
Self-management of chronic conditions such as asthma, COPD, and diabetes. Recent evidence also suggests prehabilitation is cost effective in reducing the need for surgery, reducing complications by 50% and improving recovery[4].

Establishing Shared Support and Collaborative Functions in clinical support services for systems such as:
- Regional pathology networks to deliver the recommendations of the Carter report[5] – recognising the capital funding challenge. One in three pathology networks are still running at Trust-level, despite the roadmap to service consolidation published over five years ago[6].
- Developing innovative pharmacy supply chain functions at an organisation and provider collaborative level, delivering benefits of inventory reduction, net operating cost savings and release of clinical time to care.
- Implementing collaborative procurement functions to leverage the of economies of scale and switching to evidence based lower priced products.
- Centralising sterile service functions across providers to promote standardisation and reduce operating costs.

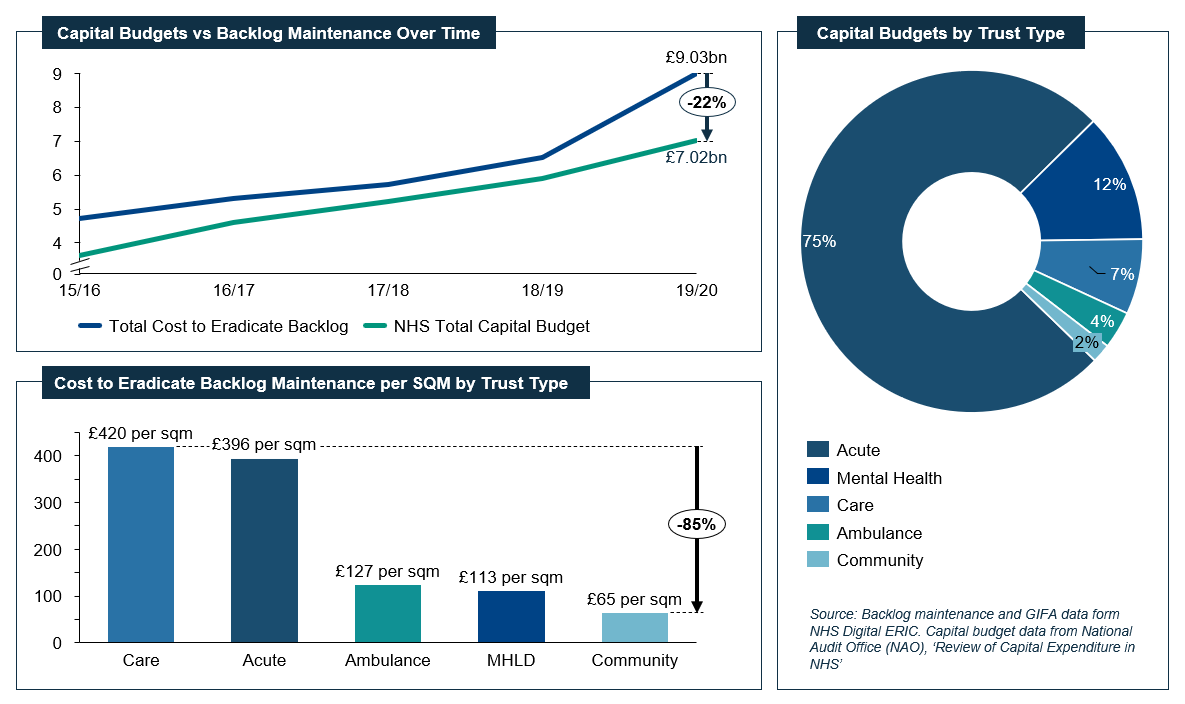
Detailed, system-wide estate planning allows organisations to work together to use their combined estate to share workloads, improve efficiencies, and reduce costs.
Examples of using a shared estate are Integrated Care Centres, to allow co-location of GP surgeries alongside other primary care facilities such as pharmacy and dental services.
Savings can also come from a system approach to the disposal of surplus properties, running costs, and backlog maintenance.
If you would like to find out more information on how Akeso can support you in delivering financial improvement schemes, please get in touch with Scott Healy, who leads our Financial Improvement offering.
The next article in our financial improvement series will focus on one of the longer-term opportunities, which is also a hot topic in public health: the role of ICBs in Population Health Management.