With an elective care backlog in excess of 7 million [1], record high workforce shortages [2] and decaying estates, our healthcare system is close to breaking point. Numerous tools have been deployed to try and combat these problems, but they continue to fall short of the mark. Not all hope is lost though. Driven by the global Covid-19 pandemic, we have seen a flurry of new techniques and solutions enter the market, promising to solve our problems and redefine healthcare nationally. One of these tools, Virtual Wards, has established such a strong base of supporting evidence that they can no longer be ignored. But are they the answer to our prayers? When deployed in a technology-enabled manner, following a structured implementation plan, they just might be.
In response to rising demand and in preparation for winter, NHS England (NHSE), Health Education England (HEE) and NHS Digital (NHSD) are collaborating to support ICSs in adopting Virtual Wards. Outlined in a two-year funded transformation program, the ambition is to have 40-50 Virtual Ward beds available in each Trust across the UK (24,000 beds in total). This is to be delivered in a tight time frame, with all Trusts required to meet the capacity target by December 2023.
With NHSE putting their faith in Virtual Wards, so too should we. But what is a Virtual Ward? What kind of benefits can they deliver and how can we ensure that our Virtual Ward is actually successful?
About Virtual Wards
Virtual Wards aren’t new, with the first examples deployed over 15 years ago [3]. At their core, they aim to move patients out of hospitals and into homes, whilst still delivering an acute level of care. Despite being used across the UK (and globally), their model of care remains largely unchanged, with little innovation or improvement seen in the space. That is, until now.
Many Virtual Wards currently in use are ‘traditional’ in their approach, with the care delivery model underpinned by telehealth services and routine home visits. This approach requires significant clinical time investment, proliferating systemic workforce problems and, in some cases, functioning to hinder the service rather than help it.
There is, however, a ‘non-traditional’ Virtual Ward model, one that uses state of the art remote monitoring technology to deliver acute level care to patients [cite]. These models are defined as ‘Technology-enabled Virtual Wards’, delivering quality care without the same workforce demand as traditional models.
Technology-enabled Virtual Wards
The NHS defines a technology-enabled Virtual Ward (TEVW) as ‘the management of patients via a digital platform’. A broad definition which could be used to describe any number of solutions currently on the market. It is also, a misleading one, as beyond the shared use of technology, there is very few similarities between the different solutions. App only, monitoring + app and telehealth platforms can all be considered as technology enabled Virtual Wards, but each has a unique set of benefits and delivers care in a novel way.
Although telehealth and app only solutions have their place, providers should be focused on deploying Virtual Wards that utilise hospital grade remote monitoring technology. These Virtual Wards are the new frontier of digital health, delivering a broader suite of benefits, to a greater patient cohort, than any other solution [4].
For the remainder of the article, when we refer to a TEVW, we refer specifically to one that is using hospital grade, remote monitoring technology.
Benefits of Technology-Enabled Virtual Wards
Not all TEVWs are built the same, with maximum (in terms of both breadth and depth) benefits only observed in those that integrate remote monitoring in patient care pathways. But what are these benefits? Where, how and by who will they be felt? To understand the potential impact of TEVW, we have conducted benefits modelling using leading technology within the Virtual ward space, Masimo SafetyNet as an example, to explore the following areas:
- Average Length of Stay
- Workforce efficiency
- Readmission rate & admission avoidance
- Backlog reduction
- Release of acute bed capacity
Our analysis models the potential positive impacts that an average sized Trust (778 beds) could achieve by adopting a TEVW. This is not the only potential application though. With appropriate tailoring, TEVWs can be applied to any use case, with the technology being used globally to support the care of patients suffering from any number of conditions from cancer to heart failure.
In the context of the acute emergency and orthopaedics cases, we understand there to be two main applications for a TEVW respectively: avoiding admission and expediting discharge. The benefits of TEVWs will be discussed in the context of these primary applications.
1) Avoiding admission
TEVWs offer providers a way to avoid unnecessary admissions and re-admissions to the acute setting, instead delivering care to patients in the home environment. Acute patients, such as emergency department attendees, can be admitted to the Virtual Ward, rather than the physical ward, preventing the occupation of an acute bed.
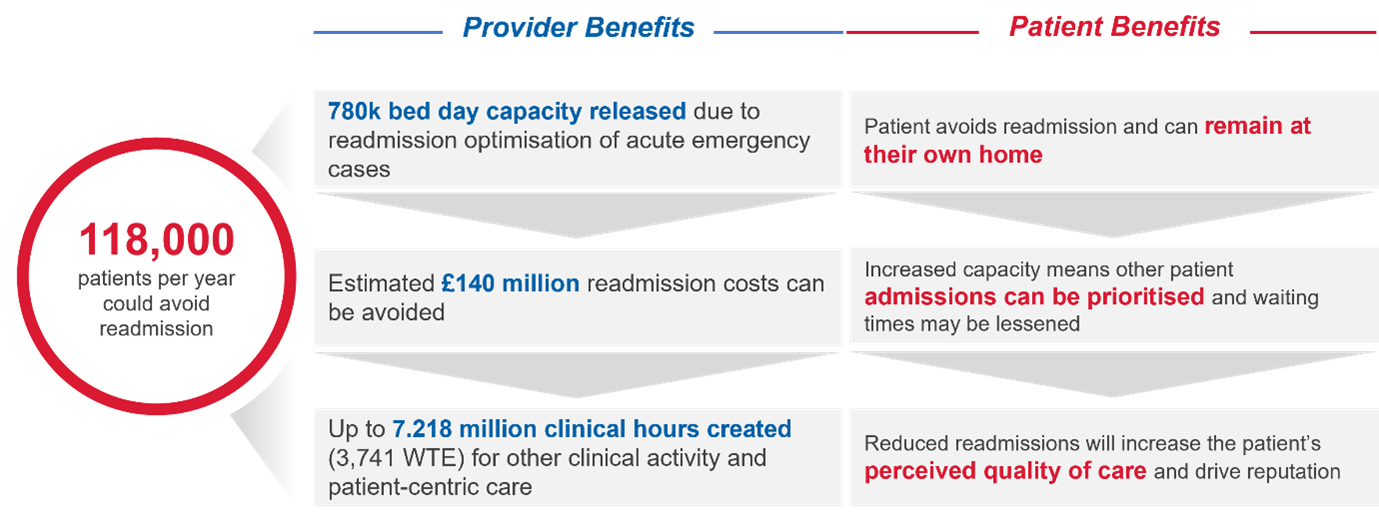
Our benefits modelling indicates that for an average sized Trust of c.760 beds, up to 7,000 bed days could be released through readmission avoidance of acute emergency patients [5,6,7,8]. This would save an estimated £3 million in avoidable readmission costs [7,9] and release 63 hours of clinical resource back to patient facing activities [10]. In addition to financial and capacity benefits, research has shown that patients have a greater perceived quality of care and sense of empowerment when treated through a TEVW model [11].
In the context of acute emergency cases:
2) Early discharge
TEVWs enable postprocedural remote monitoring and encourage early discharge, releasing both clinical and bed capacity [12,13].
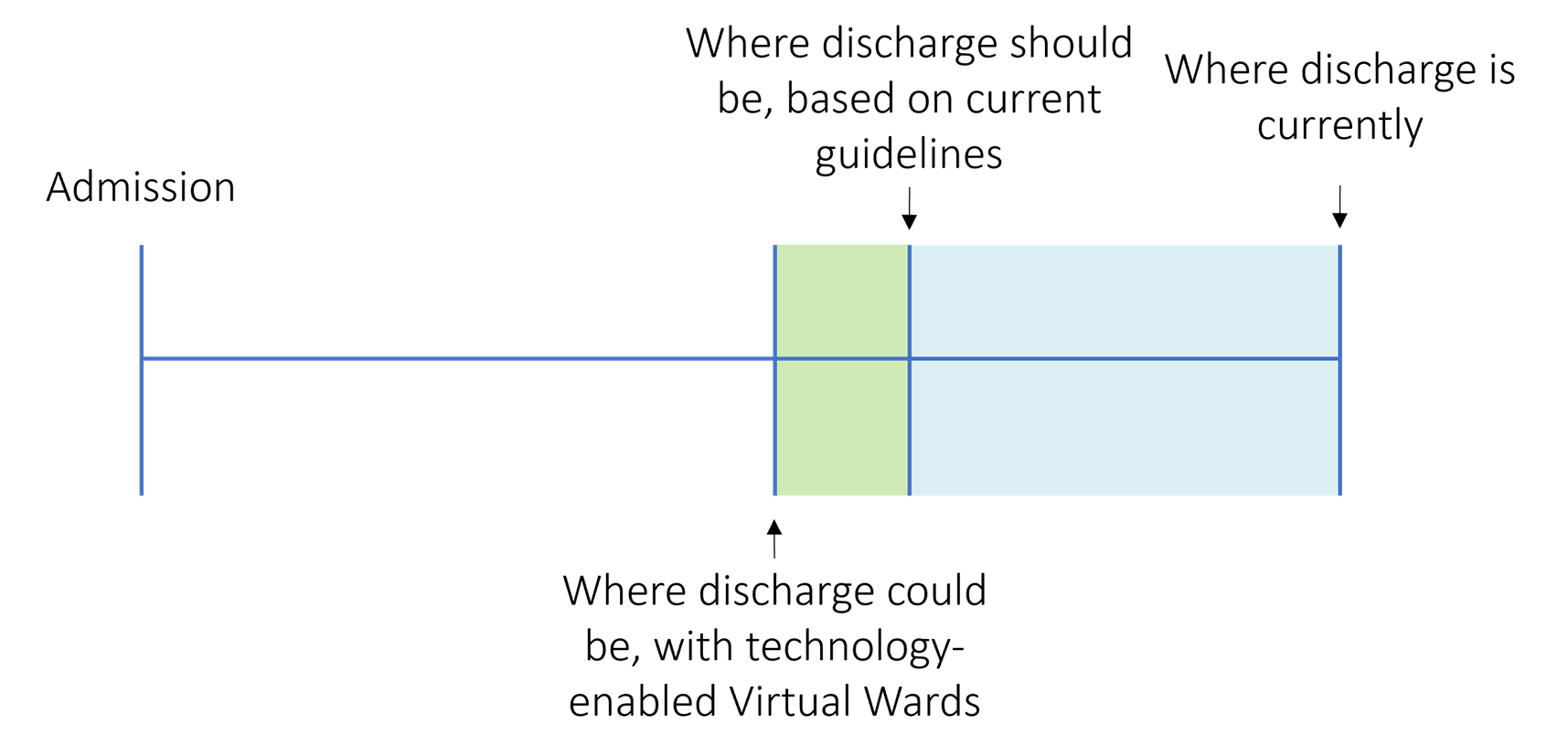
Wearable sensors alert clinicians to changes in a patient’s condition, in real-time, helping the remote management team to intervene sooner and ensuring patients receive the same quality of care within the Virtual Ward [12,13]. This functionality brings the home environment in line with the acute environment and provides clinicians with the confidence they need in order to discharge more acutely unwell individuals, earlier. 1/3 patients stay in hospital beyond the necessary point of care, the ability of TEVWs to reduce length of stay will be critical in reducing this number and expediting discharge. You can read more about this in our D2A technology article here.
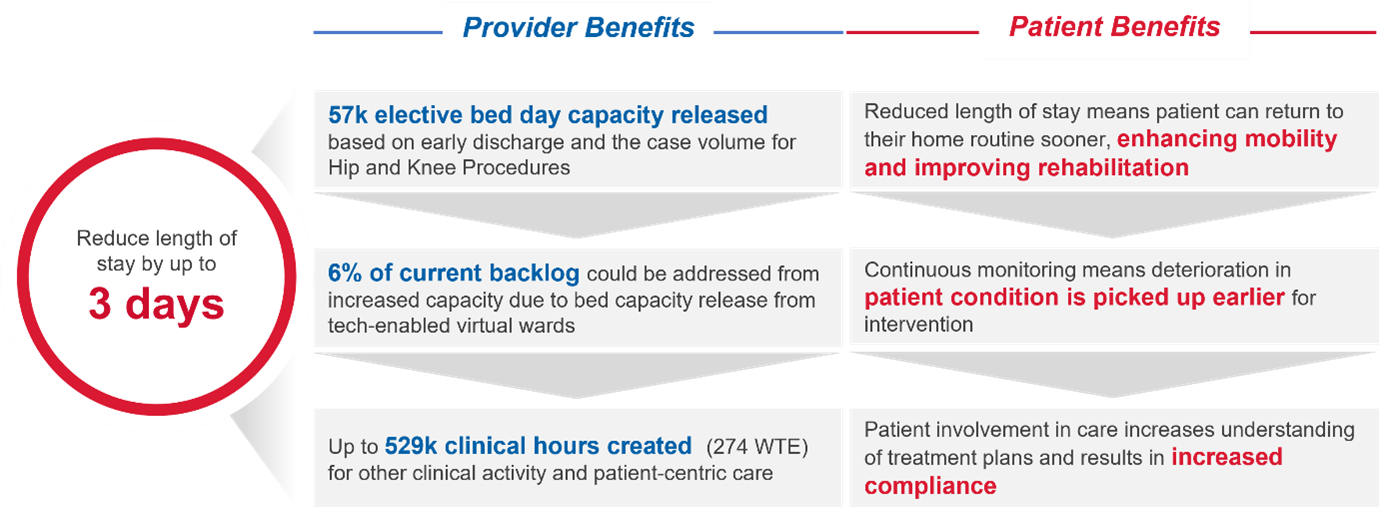
Reducing length of stay will release clinical and bed capacity, allowing critically ill patients to be treated with fewer delays and removing a key bottleneck in care delivery. In the case of primary hip and knee procedures, the ambition is that technology enabled Virtual Wards will reduce length of stay by up to 3 days. This could release an estimated 900 bed days which could be utilised to addressing the current backlog for orthopaedic procedures.
In the context of orthopaedics patients:
Implementing technology-enabled Virtual Wards
The potential benefit of technology enabled Virtual Wards is clear and as a result NHSE calling for their rapid adoption [14,15]. However, without firm guidance on how to implement these solutions effectively, they may fail to deliver expected benefits and jeopardise patient care [16].
Learnings from previous Virtual Ward implementations have been distilled into a set of critical success factors which must be considered if the TEVW is to be delivered effectively. Sourcing the right solution, defining a clear objective, mapping the commercials and understanding the use case are all pivotal in achieving success. Steps to address these factors are outlined as part of our comprehensive Virtual Ward implementation guide.
Akeso’s methodology is based on Masimo SafetyNet which you can find here.
Sourcing the right solution, and partnering with the right provider, are essential in ensuring the Virtual ward is both clinically compliant and highly effective. Several providers claim to meet these criteria, but with only a few functioning examples of TEVWs locally, it is difficult to assess the validity of these statements. route of sourcing an effective, complaint TEVW is utilise the Sparks Dynamic Purchasing System (DPS) framework. Spark DPS categorises leading technology providers across a variety of sectors based on their capabilities and offerings. We have summarised these providers, and what they offer (based on the DPS framework), below.
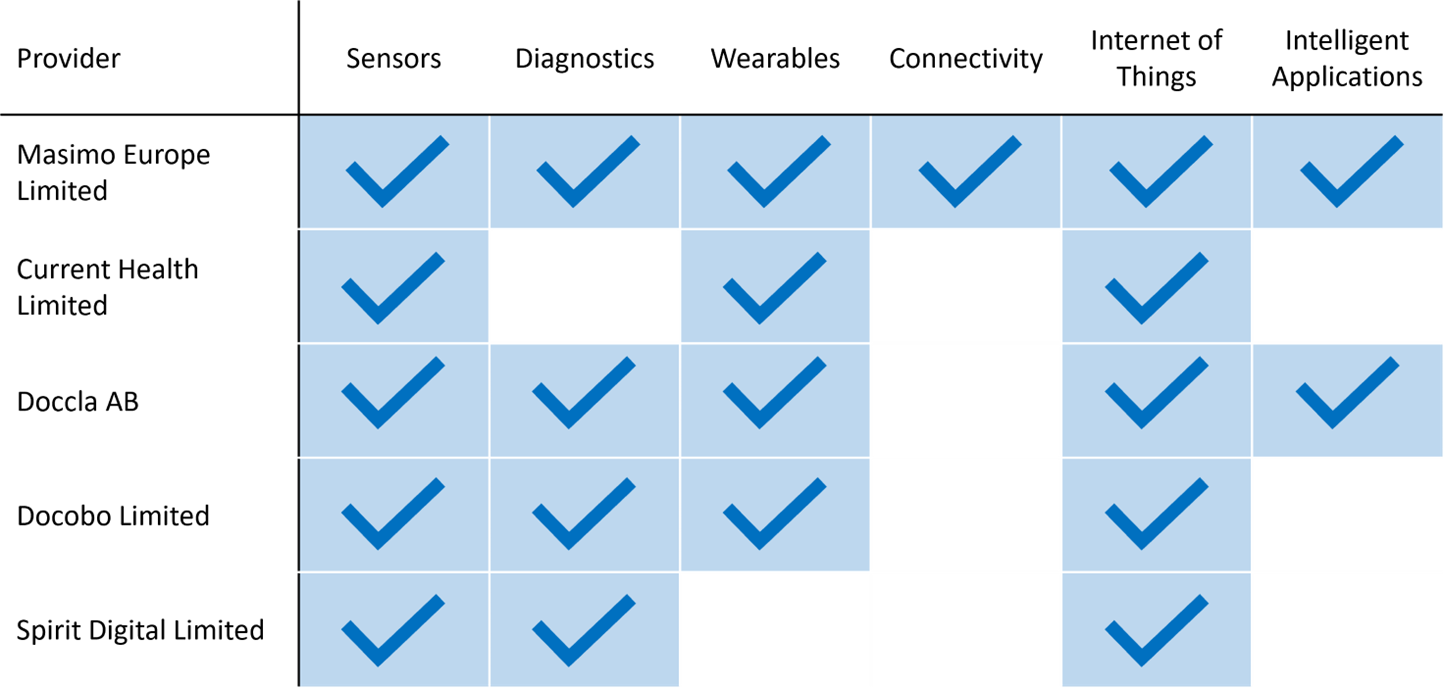
When considering which TEVW supplier to use, it is important to consider future TEVW applications, beyond the current target. Many providers have Virtual Wards up and running, supplied by different organisations. This can lead to problems with integration, consistency and quality for both patients and clinicians. The aim should be to procure a single solution that is scalable and adaptable to all areas of your service. Masimo SafetyNet is a robust example of a TEVW solution that holds this capability.
The Future
We currently have a discharge problem in the NHS, with patients waiting up to 9 months to be sent home [cite]. Virtual Wards will support expedited discharge, reducing Length of Stay back toward national targets. Read more about it in our Discharge to Assess (D2A) technology enablement article ‘Turning homes into hospitals’.
Although current benefits are obvious, we should begin to think about what role TEVWs might play in the future of healthcare. Using the clinical information TEVWs provide, we could look to begin moving the discharge threshold, allowing higher acuity patients to be treated in an at home environment. Doing so would extend the benefits of Virtual Wards, beyond what current models (including our own) predict.
But the future of Virtual Wards doesn’t just lie in moving the discharge threshold. Traditionally, Virtual Wards were deployed to prevent patient admission- the opposite end of the care pathway to the current discharge focus. We believe technology-enabled Virtual Wards could eventually be deployed across every stage of the patient care journey, not just the bookends, supporting a movement toward personalised medicine and redefining care pathways completely. There is evidence of this globally already, with Virtual Wards across Australasia supporting entire cancer care pathways [17].

It is important to keep these opportunities top of mind as we deal with our current issues, continuing to innovate and adapt during a time of immense pressure. Doing so will ensure that solutions implemented can flex and change as our needs do, remaining relevant long into the future.
References
- The British Medical Association. NHS backlog data analysis. 2022. [online] Available here.
- House of Commons Committee. Workforce: recruitment, training and retention in health and social care. 2022. [online] Available here.
- KingsFund, 2006. Case study: Virtual wards at Croydon Primary Care Trust. [ebook] Available here.
- NHSX. A guide to setting up technology-enabled virtual wards. 2022. [online] Available here.
- 15.5% avg national re-admission rate, as reported by Nuffield Trust in https://www.nuffieldtrust.org.uk/resource/emergency-readmissions
- 20% patient eligibility for MSN-enabled virtual ward, as an Akeso&Co assumption
- 6.6 days of avg length of stay for re-admission acute patients, as reported by the Internal and Emergency Medicine inhttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC8354916/
- 90% avg bed occupancy for General and Acute beds, as reported by NHSE onhttps://www.england.nhs.uk/statistics/statistical-work-areas/bed-availability-and-occupancy/bed-data-overnight/
- £400 per bed per day, 2022-23 national tariff payment system, as reported by NHSE on <https://www.england.nhs.uk/wp-content/uploads/2020/11/22-23-National-tariff-payment-system.pdf
- 1.6 WTE/bed based on avg staff required to service a 40-bedded ward in hospital published on the VW Bed Benefit Tool from NHSEI available at https://www.future.nhs.uk
- Nunan, J., Clarke, D., Malakouti, A., Tannetta, D., Calthrop, A., Hanson Xu, X., Berin Chan, N., Khalil, R., Li, W. and Walden, A., 2020. Triage Into the Community for COVID-19 (TICC-19) Patients Pathway – Service evaluation of the virtual monitoring of patients with COVID pneumonia. Acute Medicine Journal, 19(4), pp.183-191.
- Masimo. Masimo SafetyNet Telesurveillance Solution. Presentation; 2020.
- Masimo.co.uk. Masimo – About. [online] Available at: https://www.masimo.co.uk/company/masimo/about
- England.nhs.uk, 2022. Delivery Plan for Tackling the backlog of elective care. [ebook] NHS. Available at: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2022/02/C1466-delivery-plan-for-tackling-the-covid-19-backlog-of-elective-care.pdf
- NHS England, 2022. 2022/23 priorities and operational planning guidance. [ebook] Available at: https://www.england.nhs.uk/wp-content/uploads/2022/02/20211223-B1160-2022-23-priorities-and-operational-planning-guidance-v3.2.pdf
- James Illman (2022). ‘Patients at risk’ from ‘hastily rolled out virtual wards’. Health Service Journal. https://www.hsj.co.uk/quality-and-performance/patients-at-risk-from-hastily-rolled-out-virtual-wards/7031648.article
- https://theclinician.com/
