Akeso were engaged to work closely with the Clinical and Operational teams from the 9 hospitals who deliver Endoscopy Services in the ICB to model a shared waiting list for Endoscopy and identify opportunities to pool resources across neighbouring hospitals across the region to treat patients more quickly and reduce the waiting list.
INSIGHT
The demand for Endoscopy Diagnostics is increasing year-on-year driven by increases in Gastroenterology and Colorectal Surgery. As of April-24, the NHS waiting list for Gastroenterology-related Diagnostics stood at almost 170k nationally.
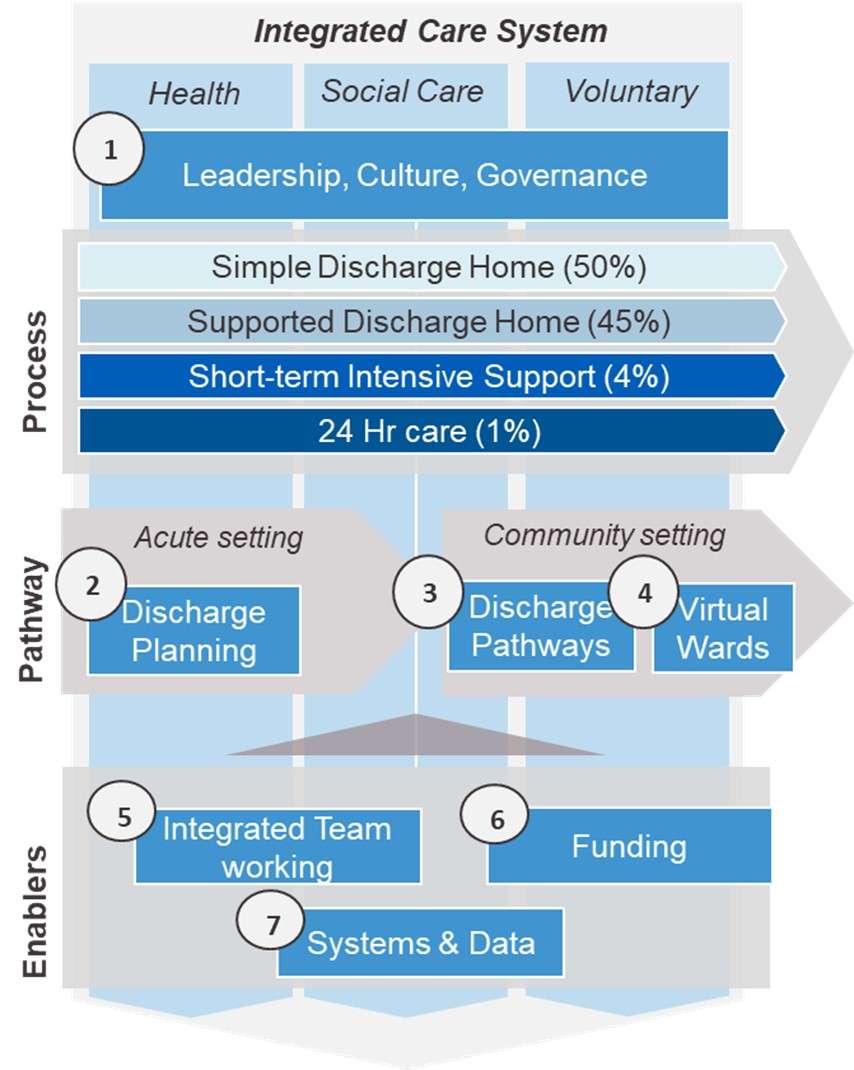
From an ICB perspective, pooling of resources across a regional Health system can be a key means to addressing the growing waiting list for a given clinical service, particularly for day case / walk in activity such as Endoscopy. It also maximises utilisation of existing resources. Our work with Health providers across the NHS suggests that capacity increases of over 20% can be achieved through pooling of waiting lists and associated resources.
To be successful however, there are a number steps that must be taken beyond the simple aggregation of the waiting list across a group of providers including: (1) building a detailed understanding the cohort of patients awaiting diagnostics / treatment, (2) understanding potential challenges and barriers to patients accessing and receiving care at an alternative provider and (3) developing strategies and plans for how these can be overcome.
ACTION
- Akeso conducted a full service ‘as-is’ review, presented through data collation, validation and analysis, which provided a network wide view of current service, including waiting lists, capacity, activity, and workforce;
- Scenario modelling was then performed utilising the current network status and changeable inputs and outputs allowing for simulation testing to understand the potentials of service optimisation, in terms of absolute waiting list reduction, additional income and costs;
- A series of business cases were then developed exploring specific options available to individual Trusts as well as the network as a whole. This incorporates options to clear the current backlogs / waiting lists, as well as how to future proof the service in accordance with demand predictions;
- A final interactive dashboard tool was developed to be used for short-medium term service planning, providing real-time service and workforce optimisation based on Trust needs.
RESULTS
We found that the ICB in question could realise a capacity increase of 20% through the pooling of waiting lists and resources. We also proposed and developed a series of recommendations, on supply and demand side, to help them address potential barriers to patients accessing available with alternative providers in the region.