-

UK Point-of-Care Market Entry Strategy
-

Virtual Ward Implementation Programme Methodology
-
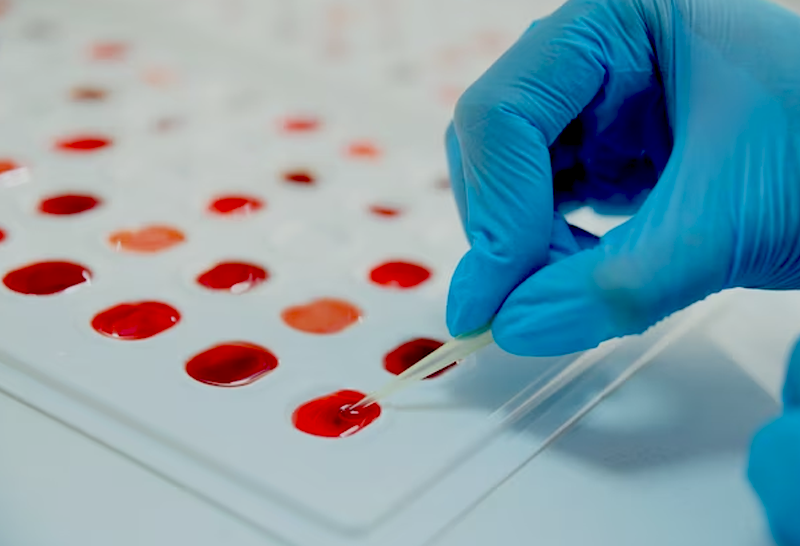
Contracting for Sample Processing in Health Research
-
Virtual Wards: First-of-kind Case Study on Heart Failure
-

Technology-enabled virtual wards the future of healthcare
-

Transforming homes into hospitals
-
Technology-enabled Virtual Wards
-

Logistics Management for a Global Pharmaceutical Company
