Sadly, recent news highlighting failures in NHS pathology diagnostics procurement will not have come as a surprise to many working in the public healthcare sector.[1] From delayed tenders to legal challenges and abandoned processes, an uncomfortable reality is becoming increasingly clear: the NHS is regularly encountering procurement challenges that cost the system not just money, but also time, trust, and, most importantly, patient outcomes.
Crucially, we understand that these challenges are not the result of failings by NHS teams themselves – but rather, the product of a system under immense pressure. Procurement, clinical and operational teams across the system are doing their best within an environment of increasing complexity, limited resources, and growing regulatory scrutiny.
At Akeso, we’ve supported NHS providers and systems through many high stakes procurements, across deeply complex and valuable services, including pathology, diagnostics, construction and estates infrastructure, as well as wider clinical support and digital services. Our team has partnered with these clients to coordinate commercial, clinical, and operational workstreams, develop technical specifications, and manage the end-to-end process from design through to evaluation. Despite the different contexts, one pattern is consistent: the challenges currently experienced are not exceptional – they are systemic, structural, and recurring.
The Current Context
NHS procurement programmes today are increasingly more important, with contracts and services often spanning decades, cutting across multiple organisations, and requiring decisions that balance cost, quality, innovation, and long-term risk. They are also becoming more collaborative in nature, with Trusts procuring major services – like pathology, EPR systems, and other diagnostic technologies, on a system-wide basis.
Whilst this collaboration adds significant value, it also creates complexity. Procurement teams must align the clinical and operational requirements of multiple Trusts and stakeholders, often with divergent needs and expectations. The structure of provider networks layered on top of Trust governance, and alongside ICB strategies, creates a fragmented environment with dispersed accountability. This misalignment often delays procurement and weakens decision-making. In our own experience, collaborative programmes are far more likely to succeed when they include deliberate and early alignment across key functions including clinical, operational, digital, estates, finance, and commercial leads. This means more than simply involving the right people; it requires establishing a shared understanding of the programme’s goals, clearly defining decision-making structures, and aligning stakeholder groups on how risks, trade-offs and benefits will be managed.
Major infrastructure procurements are particularly vulnerable due to the technical complexity involved in specification development. These programmes often involve interoperable systems that must integrate across legacy platforms, third-party solutions, and a range of clinical workflows. Notable examples stretch across multiple EPR programmes, national shared care record attempts, and regional community health service models. Consequently, the capacity of those tasked becomes a critical success factor – without it, organisations risk sub-optimally adopted systems or, in the worst cases, systems that are abandoned all together.[2]
Overlaying this is the shift in the legal landscape. The new Procurement Act, which is now in force, replaces the Public Contracts Regulations (PCR). While the fundamental principles of fairness, transparency, and value for money remain intact, procurement teams must become familiar with the updated framework and what it means in practice. The changes may not be transformational, but they introduce new obligations and a re-emphasis on transparency, making it even more important for NHS teams to be upskilled and supported during high-value procurements.
A Power Imbalance
As recent news highlights, legal challenges (whether successful or not) can derail NHS procurement. Our experience made this clear. Suppliers, often backed by dedicated legal, bid, and commercial teams, are increasingly adept at leveraging procurement regulations to their advantage. Even minor ambiguities or inconsistencies can open the door to formal challenge.[3]
This is entirely within suppliers’ rights. But when procurement teams are under-resourced and overburdened, the system creates a disproportionate burden of accountability for NHS organisations – one that drives up cost, delays delivery, and erodes confidence in local teams. The reality is that NHS buyers operate with far less legal and commercial agility than their private sector counterparts – that is, they lack the freedom to negotiate, make quick decisions, or adapt contracts when things change. This imbalance doesn’t just create friction, it distorts the procurement environment entirely. Trusts become risk-averse, decision-making slows, and the drive to deliver transformative outcomes is often replaced by a need to ‘stay challenge-proof.’
In our recent support to a major network procurement, we knew from experience how critical it was to mitigate this risk. From the outset, we built a robust documentation strategy, capturing a clear audit trail of decisions across workstreams – effectively creating a comprehensive, well-documented evidence base to support and defend the programme. On multiple occasions, we were able to dispel challenges simply by referring back to written evidence. This not only protected the programme but reinforced confidence amongst stakeholders.
In addition to the above, and one of the most significant and welcomed changes in the Procurement Act, is the specificity and focus given to preliminary market engagement; colloquially known and previously referred to as pre-market testing or soft market engagement. The encouragement to do so, and the principles supporting this, can be immensely beneficial for supporting constructive supplier relations and enabling clarity throughout the procurement process. Many procurement challenges stem from claims of unequal treatment or ambiguous specifications. When done well, early market testing can give the buyer a defensible position by demonstrating openness, fairness and robust preparation of tender materials – all of which can go a long way to reducing the likelihood of credible legal challenge.[4]
Towards a Balanced Market
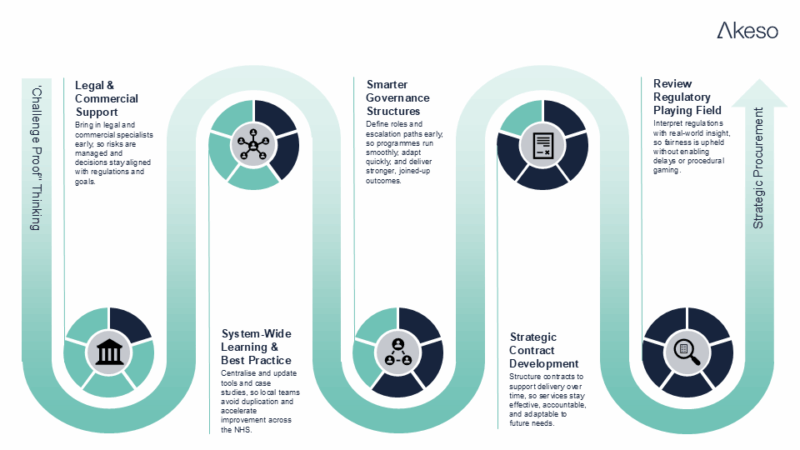
If we want to see better outcomes from major digital and infrastructure procurements, we need to move beyond an overly narrow focus on compliance, and instead build a culture of strategic and well supported decision-making. We believe five structural changes are needed to ensure NHS teams are able to operate on a more level playing field:
- Involve capable legal and commercial support early
Integrate specialist legal and commercial advisors into NHS procurement teams at the early stages of programme planning not just during crisis points. Their presence supports robust risk mitigation, ensures regulatory alignment, and strengthens commercial confidence in decision-making throughout the procurement lifecycle. - Leverage best practice and learning from across the system
Develop centralised repositories of procurement materials, including evaluation models, contract templates, and real-world case studies. Actively update and embed these resources into local practice to avoid duplication and accelerate learning across systems. - Implement smarter governance structures and agile ways of working
Establish smart governance frameworks that define clear roles, responsibilities, and escalation pathways across all involved parties. Prioritise strong leadership and agile delivery methods to enable stronger collaboration and greater overall programme management. - Design contracts with delivery and longevity in mind
Procurement doesn’t end at contract award. These contracts should be carefully structured to support long-term service delivery over the lifetime of the contract, with clear governance mechanisms, performance management frameworks, and the flexibility to adapt over time. - Review and monitor procurement regulations through a practical lens
Ensure regulation protects fairness and transparency without unintentionally enabling procedural brinkmanship. The introduction of the Procurement Act offers an opportunity to reset expectations and strike a balance that reflects the interest of all affected: both suppliers and buyers.
Conclusion
The pathology procurement challenges recently experienced are not isolated failures, but the product of a system under strain. NHS organisations are being asked to deliver transformation-level change, often without the infrastructure or tools they need to do so effectively.
Our recent work has shown that, when conditions are right, these programmes can succeed and deliver real impact. But getting there takes more than effort. It takes structural support, shared learning, legal awareness, and regulatory reform that levels the playing field.
At Akeso, we remain committed to supporting NHS Providers through this shift, not just to deliver better procurements for the contract duration, but to help build a system that is resilient in the long-term.
References
[1] Serle, J. (2025) Trusts ‘stumbling into legal challenge’ with botched procurements, Health Service Journal, 10 July. Available at: https://www.hsj.co.uk/finance-and-efficiency/trusts-stumbling-into-legal-challenge-with-botched-procurements/7039637.article
[2] BBC News. (2014) Addenbrooke’s Hospital £200m contract awarded to private firm, BBC News, 5 December. Available at: https://www.bbc.co.uk/news/uk-england-cambridgeshire-30344498
[3] NHS Procurement & Commercial Standards. (2024) Trust reverses £65m EPR procurement decision after court claim. Available at: https://www.nhsprocurement.org.uk/news/trust-reverses-65m-epr-procurement-decision-after-court-claim
[4] Hawkes, N. (2019) Judge throws out AbbVie’s case against NHS England’s hepatitis C programme, BMJ, 364, l309. Available at: https://www.bmj.com/content/364/bmj.l309

