Summary
As the new financial year approaches, planning for 2025/26 is well underway with a strong emphasis on amid significant financial challenges. A push for innovation and a less risk-averse approach is likely to be a key message in the upcoming 10-year plan, requiring the adoption of alternative interventions beyond traditional care models.
Virtual Wards (or Hospitals at Home) when effectively implemented, represent one such solution to enhance capacity through a more efficient model of care. However, with limited conclusive evidence of their benefits, thorough planning will need to navigate these uncertainties to balance the books.
In this article we look at implementation of Virtual Wards to date, addressing lessons learned to help inform operational priorities for 2025/26. In doing so, we outline practical, actionable steps for healthcare leaders looking to plan, optimise, and scale Virtual Wards, while also enabling a more holistic Virtual Care model.
Context
In April 2022, NHS England (NHSE) launched the Virtual Ward programme, allocating £450m in funding over two years as part of a drive to address capacity pressures. While the timelines1 might have lapsed, the ambition has remained clear – to continue scaling-up Virtual Wards towards an average occupancy of 80%, with the longer ambition of reaching 40-50 Virtual Ward ‘beds’ per 100,000 people.
As of December 2024, NHSE Virtual Ward Sit Rep data2 (see Figure 1) provides two views. On one hand capacity growth has stagnated at around 20 beds per 100,000—well below the 40-50 target. This is largely due to short-term funding models4 within a financially constrained system as well as variation in operations 5which has meant evidencing the impact and scaling Virtual Wards has been challenging.
On the other hand, bed occupancy is trending toward its target of 80% which would suggest increased maturity in Virtual Ward operations. As Virtual Wards continue to evolve and new insights emerge, we would anticipate this will continue to increase. However, this needs to be met with a targeted growth in capacity, enabled by funding and efficient operations, if providers are to meet next year’s productivity targets.
Average Virtual Ward Occupancy and Capacity (per 100,000 people) against national Targets
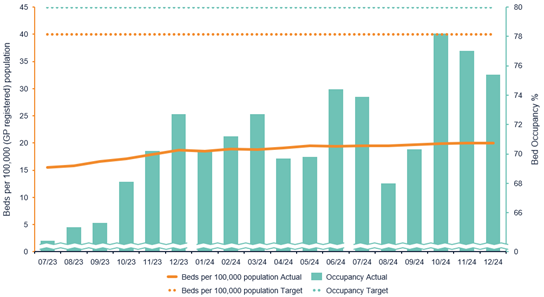
Figure 1: Whilst Virtual Ward Occupancy % is trending towards the target percentage, capacity per 100,000 GP-registered population remains far from the target, and has had little growth over the last year2
What have we learnt so far?
- Early evidence is positive – Several local case studies 8 on Virtual Wards indicate they do provide significant benefit to patient outcomes as well as financial and operational efficiencies across both specialist and general pathways. Extensive resources are continually being documented covering different pathways and themes to help build an evidence base.
- One such example is in the case of Liverpool University Hospitals NHS Foundation Trust which treated over 10,000 patients across six specialist pathways, including heart failure. Findings from a recent evaluation found an incremental net cost benefit of £735,512 (£1,135 per Patient per episode). This substantial benefit came from a reduction in length of stay as well as readmissions and unplanned contact, resulting in wider benefits to patient experience and outcome.
- Need to standardise – Deployment led by local champions is a key driver to the success of Virtual Wards to date. However, this has inevitably led to variation in services, delivery models, technology and governance structures. This inconsistency makes it challenging to effectively compare and evaluate their impact. While NHSE, with support from GIRFT, has made progress in addressing this, further consensus is needed to scale and future-proof Virtual Wards.
- Consider the whole pathway – Through our work with systems and providers, timely access to key clinical support services has proven critical to unlocking the true benefits of Virtual Wards. This includes equitable and timely access to key diagnostic testing, which can often be a barrier for patients with co-morbidities in accessing Virtual Wards. Access to other services such as Pharmacy and Homecare services is also important to ensure the patient can remain at home throughout their care.
- Virtual Wards are only the beginning – While the national direction is to move from a predominantly ‘step-down’ model to a ‘step-up’ approach, the broader ambition is to shift towards a Preventative model of care through the adoption of ‘Virtual Care’ . To distinguish the two terms, we define ‘Virtual Care’ as enhanced care provided to patients in their residence using digital technology to monitor and manage conditions for the purpose of preventing health deterioration. Using Population Health Management tools this can be advanced further to proactively stratify, identify and monitor patients. Through this approach providers can pre-empt and avoid unplanned admissions almost entirely – arguably negating the need for a patient to be referred.
- An example of where this model has been deployed successfully is with Frimley Health’s remote monitoring programme for Patients with multiple long term medical conditions. The programme which was launched in 2022 and enrolled more than 8,000 patients has found an 38.6% reduction in A&E attendances, as well as a 53.7% reduction in admissions and 26.7% reduction in outpatient appointments. Key to their integrated approach is the use of their Shared care record which provides access to wider system data including primary care records and population health data, providing Frimley with a holistic view of their population and patient needs.””
As the NHS looks to achieve the three strategic shifts in care, it’s clear that Virtual Care, in whatever form it takes, will be a key enabler to this. However, for many systems and providers, further work is required to get there. Therefore, we have set out our immediate thoughts on priorities for 2025/26.
What are the priorities for 2025/26?
- Data, Data, Data – Standardising data collection across, and between systems is the bedrock to supporting effective patient care and operational planning. Key priorities should include:
- Routine collection of patients acuity and diagnosis to track health and more easily compare Patients with inpatients.
- Robust capturing of patient, carer and staff experience- Evaluations in Bradford13 and Southwest London14 demonstrate that capturing this data can provide invaluable insight into assessing and improvement Virtual Wards.
- Data is only as good as the input provided – avoid a ‘blanket approach’. Staff and patients are more likely to input good quality data when data collection processes have been designed with the end-user in mind.
- Staff training – Our research indicates that staff satisfaction can be significantly affected if staff aren’t provided with the right support to transition between traditional and Virtual Ward care. Since Virtual Wards demand a distinct skill set, many staff members report feeling “disconnected” from patients and lacking confidence in their roles. Effective onboarding and continuous training to address skill gaps is essential for helping staff adapt to this new care model, embedding best practices, and ensuring confidence, satisfaction, and retention.
- System-wide working – Supporting the shift from hospital to home requires genuine collaboration across system partners, including community providers, GPs, and acute partners. This means designing patient pathways beyond an acute-focused model, ensuring coordinated support. System working also enables operational consolidation, as seen in the North West London Virtual Hospital, through centralised Virtual Ward administration. A single point of access could further streamline referrals, capacity management, and Advice & Guidance (A&G).
- IT Interoperability – As part of a wider digital strategy, providers should consider the integration of their Virtual Ward systems with central data repositories and shared care records to enable wider system integration and data accessibility. The long-term ambition is to to enable enhanced analytics with the use of AI and automated risk stratification.
- Population health approach – To drive a patient-centric approach and left shift in care, population heath data should be used to inform scaling and design of pathways – from accessibility of technology through to translation support. Engagement with communities is also key, a King’s Fund roundtable20 highlighted that a lack of patient input leads to exclusion. Establishing a forum to draw upon lived evidence can help to unblock barriers and ensure that Virtual Wards meet the needs of all the communities within the area.
Final Thoughts
The future of healthcare is Virtual Care, with Virtual Wards offering significant potential benefit. But to scale effectively, investment across data, system and people at both a system and provider level is essential. One thing is clear: with a 4% productivity target in a financially constrained system, providers must embrace change and take risks—and digital innovation must lead the way.
References
- https://www.health.org.uk/features-and-opinion/blogs/innovation-in-the-nhs-fixing-what-is-holding-us-back
- https://www.health.org.uk/sites/default/files/upload/publications/2024/What%20do%20virtual%20wards%20look%20like%20in%20England.pdf
- https://www.england.nhs.uk/statistics/statistical-work-areas/virtual-ward/
- https://www.nhsconfed.org/publications/realising-potential-virtual-wards
- https://www.health.org.uk/features-and-opinion/blogs/virtual-wards-no-place-like-home
- https://www.england.nhs.uk/long-read/2025-26-priorities-and-operational-planning-guidance/
- https://akeso.co.uk/case-studies/virtual-wards-performance-evaluation-re-design/
- https://future.nhs.uk/NationalVirtualWards/view?objectId=145219493
- https://www.england.nhs.uk/long-read/virtual-wards-operational-framework/
- https://gettingitrightfirsttime.co.uk/wp-content/uploads/2024/09/FINAL-Making-the-most-of-virtual-wards-September-2024-update.pdf
- https://www.england.nhs.uk/long-read/integrating-in-vitro-point-of-care-diagnostics-guidance-for-urgent-community-response-and-virtual-ward-services/
- https://www.hee.nhs.uk/sites/default/files/documents/Guidance%20on%20Pharmacy%20Services%20and%20Medicines%20Use%20within%20Virtual%20Wards%20_including%20Hospital%20at%20Home%20%281%29.pdf
- https://www.bradfordhospitals.nhs.uk/wp-content/uploads/2025/01/BTHFT-VST-Service-evaluation.pdf
- https://healthinnovationnetwork.com/wp-content/uploads/2022/11/SWL-VW-evaluation-report_final-version-21.11.22.pdf
- https://healthinnovationnetwork.com/wp-content/uploads/2022/11/SWL-VW-evaluation-report_final-version-21.11.22.pdf
- https://www.england.nhs.uk/long-read/virtual-wards-operational-framework/
- https://www.kingsfund.org.uk/insight-and-analysis/long-reads/the-reality-of-and-potential-for-digitally-enabled-care-in-the-community
