The rapid evolution of digital health technologies offers significant potential to enhance health and care delivery across global systems. The NHS Inclusive Digital Healthcare Framework, published in 2023, highlights the importance of ensuring equal access, usability, and effectiveness of digital health tools across all communities.
However, digital exclusion remains a significant issue in the UK. According to the Lloyds Bank Consumer Digital Index 2024, 16.8 million people in the UK have low or very low digital capability, limiting their ability to engage with online health and care services. Additionally, this source reveals that only 48% of the workforce can perform all 20 essential digital tasks required in modern workplaces, reflecting a significant digital skills gap.
Critically, digital exclusion does not exist in isolation—it reflects and reinforces existing social inequalities. Professor Ellen Helsper argues that digital inequalities are intertwined with education, income, and past experiences with formal institutions. Simply providing digital tools is not enough; without the skills and confidence to use them, many individuals—particularly older adults, low-income populations, and ethnic minorities—risk being left behind.
Without thoughtful implementation, digital health can deepen, rather than close, existing health disparities. This article explores the determinants of digital health inequity, the role of AI, and the steps policymakers, healthcare leaders, and tech companies must take to ensure digital transformation shrinks the inequality gap rather than widen it.
Section 1: What is health equity?
Health equity ensures that every individual has a fair opportunity to achieve their full health potential, irrespective of social, economic, or geographic disadvantages. The Marmot Review (2010) emphasises that health inequities are closely linked to social determinants of health, such as housing, education, and income.
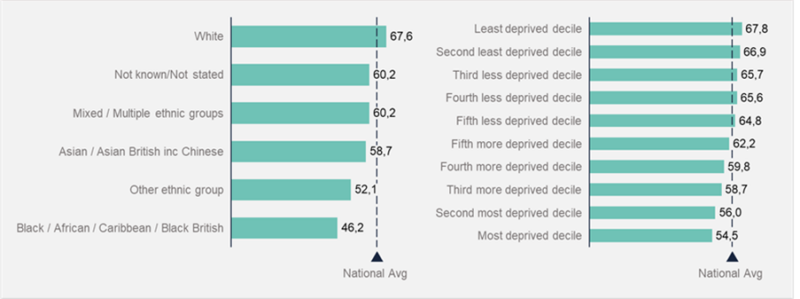
Figure 1: Shows the proportion of the population with early access to Maternity care by Deprivation Decile and Ethnic Group (Data source: Office for Health Improvement and Disparities 2022/23)
One striking example of health inequity in England is early access to maternity care (Figure 1):
- 40% of England’s population lives in areas where early access to maternity care falls below the national average (61.4%).
- White populations are above the national average for early maternity care access, while Asian and Black women experience significantly lower access.
This data highlights a socioeconomic disparity in service accessibility, which digital health technologies could help address by:
- Expanding access: Remote consultations reduce the need for travel, making it easier for pregnant women in underserved areas to receive timely care.
- Providing culturally tailored care: Digital platforms can offer language-specific resources and virtual support, addressing barriers for ethnic minority patients.
- Enhancing engagement: Pregnancy tracking apps and digital reminders encourage early and continuous prenatal care, especially for first-time mothers.
For example, a recent study found that telehealth significantly improved maternity care access for marginalised communities, enabling earlier and more frequent interactions with midwives. Similarly, Grimay (2024) showed that home-based telehealth models helped bypass geographical barriers, aligning with the community care emphasis in the Darzi Review (2024).
These findings underscore the potential of digital health to close care gaps, particularly for communities facing geographic, economic, or cultural barriers and inequalities.
Section 2: Determinants of digital health inequity
Digital health inequity is shaped by individual, systemic and structural factors—all of which must be considered when designing equitable digital solutions. Access to technology alone doesn’t guarantee improved outcomes; factors like education, socioeconomic status, and geographic location play pivotal roles.
- Individual factors:
- Digital literacy & confidence: The Lloyds Bank Consumer Digital Index 2024 found that 22.6 million people feel their digital skills need improvement.
- Affordability: Many low-income individuals cannot afford smartphones, laptops, or broadband, limiting engagement with digital health tools.
- Health literacy: Even with access to information and technology devices, understanding and applying online health advice remains a challenge for many.
- Systemic & structural barriers:
- Trust & lived experiences: LSE (2024) highlights that past experiences with formal institutions shape how people engage with digital platforms. Those who have felt alienated by healthcare systems may be less likely to use digital health services.
- Infrastructure gaps: Rural communities have 9% lower levels of superfast broadband coverage when compared to urban centres, limiting their ability to access telehealth.
- Bias in Artificial Intelligence (AI) & Healthcare Technology: Bias in digital health tools can emerge from training data, design, and human decision-making, leading to potential misdiagnoses and reduced trust in digital healthcare.
Beyond access, the delivery of digital health tools within healthcare settings is just as critical. The effectiveness of these solutions hinges on factors like the digital literacy of healthcare professionals and how well technologies are able to be integrated into existing workflows, making implementation a key determinant of health equity in the digital age.
To ensure these services are effective and equitable, it is essential to engage patients and communities in the design process. Research from the King’s Fund has shown that engagement needs to be meaningful and sustained, with a focus on addressing power dynamics and ensuring staff have the necessary support and skills to facilitate engagement. This approach helps ensure that digital health technologies are user-friendly, accessible, and tailored to the diverse needs of the whole population.
Section 3: Why AI in health and care deserves special attention
AI is one of the most powerful tools shaping the future of healthcare, with the potential to increase efficiency, personalise treatments, and reduce administrative burdens.
Opportunities of AI in digital health equity
- AI-powered translation tools help non-English speakers access NHS services, reducing language barriers.
- Adaptive user interfaces improve accessibility for those with low digital literacy, cognitive impairments, or disabilities.
- AI-driven virtual consultations enhance remote healthcare access for underserved communities.
- Risk prediction models use social determinants of health and patient data to personalise treatment recommendations, benefiting marginalised groups.
However, AI is not inherently neutral—it reflects the data, design choices, and human biases embedded within it. If developed and deployed without safeguards, AI risks amplifying existing health inequalities at scale. Training data bias is a major concern, as AI dermatology models, for instance, have been shown to misdiagnose darker skin tones at higher rates. Similarly, AI models trained on homogeneous datasets often underperform for minority populations, leading to misdiagnoses and inaccurate treatment recommendations.
To mitigate these risks, initiatives like “STANDING Together” are working to diversify AI training datasets, ensuring that AI models are built on representative, inclusive data that supports fairer and more equitable healthcare outcomes.
Section 4: Recommendations
To ensure digital health technologies reduce, rather than exacerbate, health inequalities, the NHS must take a system-wide approach that prioritises equitable access, inclusive design, and digital literacy. These recommendations build upon insights from: NHS England’s Inclusive Digital Healthcare Framework, Good Things Foundation, The King’s Fund, Johns Hopkins Public Health, and other key reports.
Government & policymakers
- Recognise digital exclusion as a determinant of health and integrate into public health strategies.
- Support initiatives, such as “STANDING Together”, that improve the diversity and inclusivity of AI training datasets to prevent bias in healthcare AI.
- Use equity impact assessments to ensure accessibility for people with disabilities and low digital literacy.
- Ensure national guidelines for AI fairness and bias mitigation are built into the AI and Digital Regulations Service for health and social care.
- Invest in community-led digital literacy learning, setting up partnerships with local charities, libraries and digital inclusion organisations to run tailored digital health workshops for those at risk of exclusion.
Healthcare systems & organisations
- Embed digital inclusion as a core pillar of their healthcare transformation strategies, ensuring all services account for digital literacy and access barriers.
- Patients, particularly from marginalised groups, must be actively involved in designing digital services. Digital health technologies should be co-developed with users, through on-going and meaningful engagement.
- Not all patients can access digital-first healthcare, so phone, postal, and in-person NHS services must remain available. A hybrid approach offering services with different levels of digitalisation helps to flex around people’s preferences.
- Fund training for staff on digital health technologies, ensuring effective adoption, and on how to facilitate patient engagement.
Tech & digital health companies
- Develop and implement digital health solutions that consider the diverse needs of all users, reducing and eliminating barriers to access.
- Engage in meaningful and ongoing engagement with diverse patient groups to ensure technologies are user-friendly and accessible.
- Companies working with NHS data should audit AI models regularly for bias and train algorithms on diverse datasets to improve equity.
- Digital tools must integrate across primary, secondary, community and social care systems to avoid fragmentation of care.
Section 5: How Akeso supports digital health equity
At Akeso, we use data-driven insights to help health and care organisations tackle digital exclusion. Our Population Health Clustering tool analyses socio-demographics, health outcomes, and healthcare access patterns to identify communities most at risk of digital exclusion.
Included in the tool is the Digital Exclusion Risk Index, produced by the Greater Manchester Combined Authority, which is calculated from demography, deprivation and broadband access. By pinpointing communities at the highest risk of digital exclusion, we can help NHS partners and ICSs design digital health strategies and solutions, ensuring digital transformation works for everyone, not just the digitally literate.
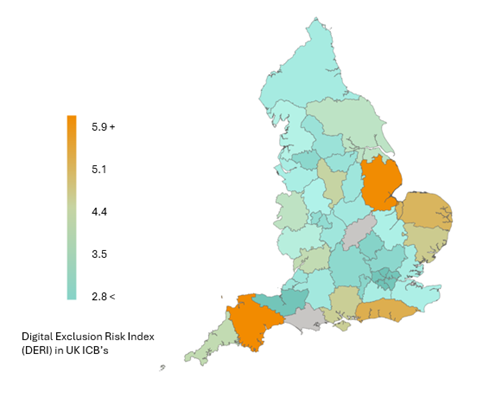
Figure 2: Presents the Digital Exclusion Risk Index (DERI) across Integrated Care Boards (ICBs) in England, calculated using data sourced from the Office for National Statistics (ONS) and Census data. The index highlights areas with varying levels of digital exclusion risk, reflecting factors such as broadband access, digital literacy, and socioeconomic indicators. ICBs shown in grey did not meet the minimum data requirements necessary to calculate a DERI score.
Conclusions
Digital health transformation presents an unprecedented opportunity to improve healthcare accessibility, efficiency, and personalisation. However, without thoughtful implementation, it risks reinforcing, rather than reducing, existing health inequalities. Digital exclusion is not just about access—it reflects deeper social, economic, and systemic disparities that must be addressed through coordinated efforts from government, healthcare systems, and technology developers. By taking a system-wide, equity-driven approach, the NHS, policymakers, and digital health companies can ensure that innovation leads to better health outcomes for all.
To read more about our Digital Transformation work click here.
References
- Celeste, C., Ming, D., Broce, J. et al. Ethnic disparity in diagnosing asymptomatic bacterial vaginosis using machine learning. npj Digit. Med. 6, 211 (2023). https://doi.org/10.1038/s41746-023-00953-1
- Darzi, A. (2024) Independent investigation of the NHS in England, GOV.UK Department of Health and Social Care. Available at: https://www.gov.uk/government/publications/independent-investigation-of-the-nhs-in-england.
- Department of Health and Social Care (DHSC) (no date) Child and maternal health: Fingertips: Department of Health and Social Care, Fingertips Public Health Profiles. Available at: https://fingertips.phe.org.uk/profile/child-health-profiles.
- Diwakar, V. and Owolabi, B. (2025) Tackling digital exclusion and health literacy: How libraries can help bridge the gap, NHS England. Available at: https://www.england.nhs.uk/blog/tackling-digital-exclusion-and-health-literacy-how-libraries-can-help-bridge-the-gap/.
- Girmay M. Digital Health Divide: Opportunities for Reducing Health Disparities and Promoting Equitable Care for Maternal and Child Health Populations. Int J MCH AIDS. 2024 Dec 20;13:e026. doi: 10.25259/IJMA_41_2024. PMID: 39776789; PMCID: PMC11705165.)
- Good Things Foundation (no date) Fixing the digital divide: Good things foundation, Good Things Foundation. Available at: https://www.goodthingsfoundation.org/.
- Greater Manchester Combined Authority (no date) Digital Exclusion Risk Index (DERI), Greater Manchester Combined Authority. Available at: https://www.greatermanchester-ca.gov.uk/what-we-do/digital/get-online-greater-manchester/greater-manchester-wide-support/digital-exclusion-risk-index-deri/
- Helsper, E. and Nixon, D. (2024) How to address ‘Digital’ inequalities, LSE. Available at: https://blogs.lse.ac.uk/inequalities/2024/02/21/how-to-address-digital-inequalities/.
- John Hopkins (2025) Bridging the digital divide in health care: A new framework for Equity, Johns Hopkins Bloomberg School of Public Health. Available at: https://publichealth.jhu.edu/2025/bridging-the-digital-divide-in-health-care-a-new-framework-for-equity.
- Kamulegeya, L.H. et al. (2019) Using artificial intelligence on dermatology conditions in Uganda: A case for diversity in training data sets for machine learning [Preprint]. doi:10.1101/826057.
- Marmot, M. (2010) Fair Society, healthy lives : The marmot review : Strategic review of health inequalities in England post-2010., GOV.UK. Available at: https://www.gov.uk/research-for-development-outputs/fair-society-healthy-lives-the-marmot-review-strategic-review-of-health-inequalities-in-england-post-2010
- Massachusetts General Hospital (2023) Toolkit for Digital Health Equity, PCORI. Available at: https://www.pcori.org/engagement/engagement-resources/toolkit-digital-health-equity.
- Mistry, P. and Jabbal, J. (2023) Moving from exclusion to inclusion in digital health and care, The King’s Fund. Available at: https://www.kingsfund.org.uk/insight-and-analysis/long-reads/exclusion-inclusion-digital-health-care.
- Mittermaier, M., Raza, M. and Kvedar, J. (2023) Bias in AI-based models for medical applications: Challenges and mitigation strategies, Nature. Available at: https://www.nature.com/articles/s41746-023-00858-z.
- NHS (no date) Understanding regulations of AI and digital technology in health and social care, NHS AI and Digital Regulations Service for health and social care. Available at: https://digitalregulations.innovation.nhs.uk/.
- NHS AI Lab (no date) Machine Learning for Healthcare 2024, Standing Together. Available at: https://www.datadiversity.org/ml4hc2024.
- NHS England (2023) Inclusive digital healthcare: a framework for NHS action on digital inclusion, NHS England. Available at: https://www.england.nhs.uk/long-read/inclusive-digital-healthcare-a-framework-for-nhs-action-on-digital-inclusion/.
- Ofcom (2024) Full-fibre broadband reaches nearly 7 in 10 homes, Ofcom. Available at: https://www.ofcom.org.uk/phones-and-broadband/coverage-and-speeds/full-fibre-broadband-reaches-nearly-7-in-10-homes/.
- Shah DA, Sall D, Peng W, Sharer R, Essary AC, Radhakrishnan P. Exploring the role of telehealth in providing equitable healthcare to the vulnerable patient population during COVID-19. Journal of Telemedicine and Telecare. 2024;30(6):1047-1050. doi:10.1177/1357633X221113711
- Wills, E., Mistry, P. and Gowar, C. (2025) Designing inclusive and trusted digital health services with people and Communities, The King’s Fund. Available at: https://www.kingsfund.org.uk/insight-and-analysis/long-reads/inclusive-digital-services-people-communities.
- Wilson, S. et al. (2024) ‘Recommendations to advance digital health equity: A systematic review of qualitative studies’, npj Digital Medicine, 7(1). doi:10.1038/s41746-024-01177-7.
- Xiaoxuan, L. and Alderman, J. (2024) New recommendations to increase transparency and tackle potential bias in medical AI Technologies, University of Birmingham. Available at: https://www.birmingham.ac.uk/news/2024/new-recommendations-to-increase-transparency-and-tackle-potential-bias-in-medical-ai-technologies#:~:text=Innovative%20medical%20AI%20technologies%20may,people%20and%20not%20for%20others
